BT474 xenograft model
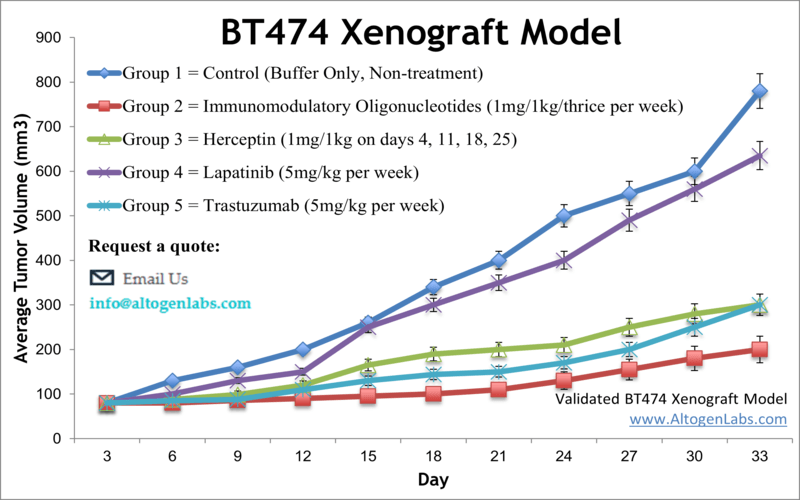
Invasive ductal carcinoma represents the most common form of breast cancer and is found in about 80 percent of all breast cancer cases. Despite significant improvements in breast cancer management and diagnosis, early detection of breast cancer plays an essential role in the overall treatment. Preclinical studies of the BT474 mouse xenograft model can be used to evaluate anti-cancer therapies. Well-studied breast tumor cell lines are indispensable tools for investigating cell biology of carcinomas. Breast cancer cell lines are extensively employed in preclinical research as molecular models of different types of breast tumors. The BT474 tumorigenic epithelial cell line is isolated by E. Lasfargues and W.G. Coutinho from a solid, invasive ductal carcinoma of the human breast of a 60-year-old Caucasian female patient. The BT474 cell line is aneuploid with a modal chromosome number of 55, as indicated in a 1978 article in Journal of the National Cancer Institute. The BT474 cell line is used to create the CDX (Cell Line Derived Xenograft) BT474 xenograft mouse model. The BT474 breast cancer model can be used to screen anti-cancer therapeutics related to the standard of care drugs (herceptin, lapatinib, trastuzumab) or hormone-induced disease progression (progesterone, norgestrel, norethindrone and MPA).
Examples include the 2015 OncoImmunology study (Zhang et al.) that used the BT474 model to investigate acquired resistance against trastuzumab and develop novel human epidermal growth factor 2 (HER2) antibodies. Their data suggested that blocking the HER2 protein could trigger calreticulin exposure and subsequently cause tumor specific T cell immunity which decreases tumor recurrence. A 1995 study (Slooten et al.) established BT474 as a powerful model for hormone-dependent breast cancer and immune therapy as these cells are oestrogen receptor positive and overexpress c-ErbB-2 protein (more commonly known now as HER2) with the in vivo phenotype of poorly differentiated adenocarcinoma that have high proliferative and turnover rate.
BT474 Breast Cancer Orthotopic And Metastatic Xenograft Model: Download ![]()
Download Altogen Labs BT474 Xenograft Model PowerPoint Presentation: ![]()
The Metastatic BT474 Model and Investigating HER2-Positive Cancer Spread
The metastatic BT474 model is a preclinical xenograft model used to study the metastasis of HER2-positive breast cancer. In this model, BT474 cells, which overexpress the HER2 receptor, are injected orthotopically into the mammary fat pad of immunocompromised mice, such as NCr-nu/nu or NSG mice. This approach allows for the observation of primary tumor growth, as well as the potential for metastatic spread to distant organs, including the lungs, liver, and lymph nodes. The metastatic BT474 model is particularly valuable for understanding the biology of tumor dissemination and investigating therapeutic strategies aimed at preventing or reducing metastasis. Researchers can track tumor growth and metastasis through imaging techniques, such as caliper measurements, bioluminescence, or histological analysis. The model enables the evaluation of various therapies, including targeted treatments, chemotherapy, and novel agents designed to inhibit metastasis. By studying the metastatic potential of BT474 tumors, this model provides crucial insights into tumor progression, resistance mechanisms, and the efficacy of therapies in reducing metastatic burden. Overall, the metastatic BT474 model offers a critical platform for cancer research focused on metastasis and therapeutic development.
Studying Tumor Growth and Metastasis with the Orthotopic BT474 Model
The orthotopic BT474 model is a preclinical xenograft model that closely mimics human breast cancer by implanting BT474 cells directly into the mammary fat pad of immunocompromised mice, such as NCr-nu/nu or NSG mice. This model is particularly valuable for studying the progression of HER2-positive breast cancer, as BT474 cells overexpress the HER2 receptor, which is a key target in targeted therapies. The orthotopic approach better recapitulates the tumor microenvironment and metastasis patterns seen in human breast cancer, providing more clinically relevant data. Tumor growth is monitored through imaging techniques such as caliper measurement or bioluminescence, with tumor progression tracked over time. The model enables researchers to evaluate the efficacy of various treatments, including chemotherapy, targeted therapies, and immunotherapies, specifically tailored to HER2-positive tumors. Additionally, the orthotopic BT474 model allows for the study of tumor invasion and metastasis to distant organs, such as the lymph nodes, lungs, and liver, making it essential for investigating metastasis and therapeutic response. This model provides insights into both primary tumor growth and the potential for secondary spread, making it an invaluable asset for drug development and cancer research.
Basic study design
- BT474 cells for injection are maintained under aseptic conditions of exponential growth prior to injection.
- Cells are trypsinized and cell count viability is determined using a trypan blue exclusion assay (98% of cell viability is required). BT474 cell suspension is adjusted to appropriate density.
- Each mouse (NSG, 12 w.o.) receive a single subcutaneous injection into the right flank area containing one million cells in a volume of 100 microliters of a Matrigel-BT474 cell suspension.
- The injection sites are palpated up to three times weekly until tumors are established. Tumors are then measured via digital calipers until an average size of 200-250 mm3 is established.
- Animals are then randomized into appropriate treatment cohorts and administration of test compound is performed according to the established treatment schedule.
- Mouse weights are recorded 3 times weekly and tumors are measured daily.
- End of study is reached when tumor size reaches 2,000 mm3 or the predetermined size limit per approved IACUC protocol.
- Final necropsy and tissue collections are performed as defined for termination of experiment.
- Tumors are excised, weighed and documented by digital imaging
- Gross necropsies are performed and tissues are collected for downstream analysis.
- Tumors and tissues can be stabilized in RNAlater, snap frozen in LN2or prepared for histology.
Get Instant Quote for
BT474 Xenograft Model
Understanding BT474: Sensitivity and Resistance in Breast Cancer Treatment
BT474 is a human breast cancer cell line that overexpresses the HER2/neu (ErbB2) receptor, making it a model system for studying HER2-positive breast cancer. It has been extensively used to investigate the effects of targeted therapies, including trastuzumab, pertuzumab, and the tyrosine kinase inhibitor lapatinib. Studies show that trastuzumab effectively induces cell-cycle arrest in BT474 cells, though resistance mechanisms can emerge. The presence of epidermal growth factor (EGF) or heregulin (HRG) can counteract the growth inhibition effects of targeted therapies, emphasizing the complexity of HER2 signaling. Lapatinib is a potent inhibitor of BT474 cell proliferation, but its effectiveness can be diminished by compensatory signaling from growth factors. Combining multiple HER2-targeting agents, such as trastuzumab, pertuzumab, and lapatinib, has been shown to enhance therapeutic efficacy. These findings highlight the need for combination therapies and personalized treatment approaches to overcome drug resistance in HER2-positive breast cancer.
BT474 Breast Cancer Model Validates Dual PIM/PI3K Inhibition as a Novel Therapy
Study performed by Kennedy SP and colleagues and published in Oncogene journal, evaluates the preclinical efficacy of IBL302, a novel inhibitor targeting PIM and PI3K/mTOR pathways, in breast cancer models, including HER2+ and trastuzumab-resistant cell lines. BT474, a HER2+/PIK3CA-mutated breast cancer cell line, was used extensively in both in vitro and in vivo assessments. IBL302 effectively inhibited tumor growth in BT474 xenografts, demonstrating significant reductions in tumor volume compared to controls. Mechanistically, IBL-302 suppressed key survival pathways by reducing phosphorylation of AKT, mTOR, and BAD, thereby inducing apoptosis in BT474 cells. Additionally, combining IBL302 with trastuzumab enhanced the anti-proliferative effect, even in trastuzumab-resistant BT474 variants, supporting its role in overcoming resistance mechanisms. In vivo, BT474 xenograft tumors treated with IBL-302 exhibited notable tumor regression, reinforcing its therapeutic potential. These findings suggest that dual inhibition of PIM and PI3K/mTOR pathways using IBL302 could be a promising approach for treating HER2+ breast cancer, particularly in patients with resistance to existing therapies.
BT474 Breast Cancer Cells: A Model for HER2-Driven Tumorigenesis
BT474 is a well-established human breast cancer cell line derived from an invasive ductal carcinoma. It is characterized by strong overexpression of the c-ErbB-2 (HER2/neu) oncogene, a feature observed in approximately 30% of human breast cancers. This overexpression is associated with increased tumorigenicity, resistance to apoptosis, and potential resistance to anti-estrogen therapies. Unlike many other HER2-positive cell lines, BT474 is also estrogen receptor (ER)-positive, making it a valuable model for studying hormone-dependent breast cancer. In vivo, BT474 tumors exhibit high proliferative activity but also undergo significant apoptosis, likely influenced by Bcl-2 expression and the absence of wild-type p53. These tumors are capable of metastasizing to regional lymph nodes and forming micro-metastases in the lungs. The dual expression of HER2 and hormone receptors makes BT474 an essential model for testing targeted therapies, including HER2 inhibitors, endocrine therapies, and novel combination treatments.
Following options are available for the BT474 xenograft model:
- BT474 Tumor Growth Delay (TGD; latency)
- BT474 Tumor Growth Inhibition (TGI)
- Dosing frequency and duration of dose administration
- Dosing route (intravenous, intratracheal, continuous infusion, intraperitoneal, intratumoral, oral gavage, topical, intramuscular, subcutaneous, intranasal, using cutting-edge micro-injection techniques and pump-controlled IV injection)
- BT474 tumor immunohistochemistry
- Alternative cell engraftment sites (orthotopic transplantation, tail vein injection and left ventricular injection for metastasis studies, injection into the mammary fat pad, intraperitoneal injection)
- Blood chemistry analysis
- Toxicity and survival
- Gross necropsies and histopathology, toxicology
- Positive control group employing cyclophosphamide, at a dosage of 50 mg/kg administered by intramuscular injection to the control group daily for the study duration
- Lipid distribution and metabolic assays
- Imaging studies: Fluorescence-based imaging, biodistridution
