Breast cancer is one of the most common malignancies affecting people worldwide, with significant challenges in treatment and disease progression. Researchers often use xenografts, tumor models created by transplanting human breast cancer cells into immunocompromised mice to study the disease in a controlled environment. These models closely mimic human tumor behavior, allowing scientists to investigate tumor growth, metastasis, and response to therapies. Cell line-derived xenografts (CDXs), established from cultured breast cancer cell lines, provide a reproducible and widely used platform for studying tumor biology and drug efficacy. Patient-derived xenografts (PDXs), in particular, retain the genetic and histological characteristics of the original tumor, making them valuable for personalized medicine research. By using xenografts, scientists can test new drugs, explore resistance mechanisms, and develop targeted therapies.
SUM185 Breast Cancer Xenograft Model: Download ![]()
SUM185PE Cell Line
The SUM185PE cell line is an immortalized breast cancer cell line derived from the pleural effusion of a patient diagnosed with anaplastic carcinoma of the breast. This cell line is characterized by its ER-negative, PR-negative, and HER2-positive status, making it a valuable model for studying HER2-driven breast cancers. SUM185PE cells overexpress HER2, which plays a critical role in their proliferation and survival, making them particularly useful for investigating HER2-targeted therapies. Additionally, these cells express luminal cytokeratin 8, 18, and 19, indicating their origin from luminal breast epithelial cells. The expression of these cytokeratin suggests that SUM185PE cells retain characteristics of luminal differentiation, despite their aggressive nature. As an immortal cell line, SUM185PE can be continuously cultured, providing a stable platform for experimental reproducibility. Researchers frequently utilize this model to explore HER2-targeted drug responses, resistance mechanisms, and tumor biology. Given its molecular profile, SUM185PE is often utilized in the development of novel therapeutic strategies for HER2-positive breast cancer.
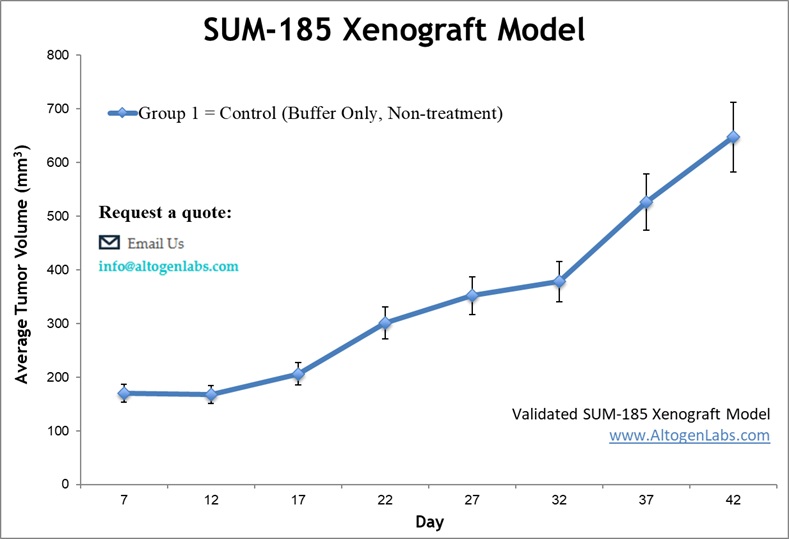
The subcutaneous SUM185PE xenograft model is a widely used preclinical system for studying HER2-positive breast cancer in vivo. In this model, SUM185PE cells are injected under the skin of immunocompromised mice, such as athymic BALB/C or NOD/SCID mice, typically in the hind legs. This allows for the controlled assessment of tumor growth, drug response, and molecular characteristics. The cells are typically suspended in a 1:1 mixture with Matrigel to enhance tumor engraftment and maintain structural integrity. Tumor development is monitored using digital calipers, with regular measurements taken to evaluate growth kinetics and treatment efficacy.
Orthotopic Model
The orthotopic SUM185PE xenograft model provides a biologically relevant system for studying HER2-positive breast cancer by implanting SUM185PE cells directly into the mammary fat pad of immunocompromised mice. This approach allows the tumor to develop in its native microenvironment, preserving critical cellular interactions, stromal components, and signaling pathways that influence tumor progression. Tumor engraftment is typically enhanced by suspending SUM185PE cells in a Matrigel mixture, promoting structural integrity and vascularization. Growth is monitored using digital calipers, while additional imaging techniques, such as bioluminescence or ultrasound, can be used to track tumor development and response to therapy. This model is particularly useful for evaluating HER2-targeted therapies, studying tumor-stroma interactions, and assessing local invasion and metastatic potential. Compared to subcutaneous models, orthotopic xenografts more accurately reflect the tumor microenvironment, making them ideal for investigating therapeutic resistance mechanisms and drug efficacy.
Genomic Instability and Oncogenic Drivers in the SUM185PE TNBC Model
The SUM185PE cell line exhibits a highly aneuploid karyotype, with an abnormal number of chromosomes; characterized by multiple chromosomal aberrations, gains, and losses, which contribute to its aggressive nature as a luminal androgen receptor (LAR)-positive triple-negative breast cancer (TNBC) model. Notably, chromosome 8q gains are frequently observed, leading to the overexpression of oncogenes like MYC, which drives tumor progression. Additionally, loss of 8p and 17p, particularly deletions affecting TP53, disrupts genomic stability and impairs DNA damage response mechanisms. The PIK3CA gene, located on chromosome 3q, is often amplified or mutated in SUM185PE, enhancing PI3K/Akt/mTOR signaling, a key pathway for tumor cell survival and proliferation. Structural abnormalities, including chromosomal translocations and copy number variations, further contribute to oncogenic activation and therapy resistance. The presence of these widespread karyotypic alterations suggests that SUM185PE cells may be particularly sensitive to PI3K/mTOR inhibitors and AR-targeted therapies, providing insights into potential therapeutic strategies for AR-positive TNBC subtypes.
Inhibition of AR and Chemotherapy Resistance in TNBC with Ceritinib
In a study by Dong S, et al., published by Molecular Cancer journal, researchers identified ceritinib as an effective therapeutic agent against SUM185PE, a luminal androgen receptor (LAR)-positive triple-negative breast cancer (TNBC) cell line. Ceritinib inhibits the RTK-ACK1-AR pathway, blocking both androgen-dependent and androgen-independent AR signaling, a key driver of tumor growth in SUM185PE. The drug also suppresses FAK-YB-1 signaling, overcoming resistance to chemotherapy agents like paclitaxel. A combination of ceritinib and enzalutamide (an AR antagonist) significantly reduced tumor growth in SUM185PE xenograft models, demonstrating a synergistic effect in targeting AR-positive TNBC. Additionally, ceritinib enhances the efficacy of paclitaxel in AR-negative and AR-low TNBCs, offering a broader therapeutic potential. Mechanistic studies revealed ceritinib’s ability to downregulate HER2, HER3, and WNT/β-catenin signaling, pathways associated with cancer stem cell maintenance and metastasis. These findings highlight ceritinib as a promising targeted therapy for LAR TNBC, particularly when used in combination with AR inhibitors or chemotherapy.
Selective Cytotoxicity of Deguelin in SUM185PE Breast Cancer Cells
A study by Robles AJ, et al., published by Breast Cancer Research and Treatment journal identifies deguelin, a natural compound, as a selective inhibitor of luminal androgen receptor (LAR)-positive triple-negative breast cancer (TNBC), specifically affecting SUM185PE and MDA-MB-453 cells. SUM185PE cells, a model for LAR TNBC, showed significant growth inhibition, demonstrating high selectivity compared to other TNBC subtypes. Deguelin inhibits the PI3K/Akt/mTOR signaling pathway and reduces androgen receptor (AR) levels and nuclear localization, suggesting a dual mode of action. Furthermore, deguelin’s effects on AR degradation resemble those of Hsp90 inhibitors, indicating a potential vulnerability in AR-driven breast cancers. Researchers also observed inhibition of mTORC1 signaling, particularly through suppression of ribosomal protein S6 (RPS6) phosphorylation, suggesting a key role in SUM185PE cell survival. Based on these findings, researches propose that combining mTOR inhibitors (rapamycin) with antiandrogens (enzalutamide) may offer an effective therapeutic strategy for AR-positive TNBC, including SUM185PE tumors.
Targeting PI3K Pathway Dependency in SUM185PE
The SUM185PE cell line is a model for luminal androgen receptor-positive (LAR) triple-negative breast cancer (TNBC), a subtype that relies on androgen receptor (AR) signaling rather than estrogen or progesterone receptors for growth. It exhibits hyperactivation of the PI3K/Akt/mTOR and MAPK pathways, making these key therapeutic targets. This cell line is particularly sensitive to PI3K inhibitors like wortmannin, as its proliferation is highly dependent on PI3K catalytic activity. Additionally, SUM185PE cells show a strong correlation between MEK and PI3K activity, indicating significant crosstalk between these pathways. Experimental treatments have demonstrated that targeting PI3K signaling leads to substantial tumor growth inhibition, highlighting the potential of PI3K inhibitors for this TNBC subtype. Xenograft studies confirm that SUM185PE tumors respond to wortmannin but are resistant to MEK inhibition, reinforcing the importance of PI3K pathway dependency. Understanding these molecular vulnerabilities could aid in developing precision therapies for LAR-positive TNBC, particularly for patients who do not benefit from standard TNBC treatments.
Harnessing Organoids to Study Tumor Heterogeneity and Drug Resistance
Organoids are three-dimensional cultures derived from patient tumor samples that retain the genetic and phenotypic diversity of the original tumor. Unlike traditional 2D cell cultures, organoids preserve complex tissue architecture and can be efficiently expanded from primary patient material, making them essential for personalized cancer research and drug testing. While xenograft and allograft models involve implanting tumors into animals to study tumor-stroma and immune interactions, organoids provide a faster and more scalable platform for assessing therapeutic responses in vitro. These models mimic the native tissue microenvironment and offer greater efficiency and reproducibility compared to animal models. Advances in organoid technology have led to the creation of patient-derived tumor organoid (PDTO) biobanks, acting as living resources to investigate cancer progression, drug resistance, and personalized medicine. Organoids are particularly useful for high-throughput drug screening, enabling researchers to identify potential treatments tailored to individual tumor profiles. They are also ideal for studying mechanisms of drug resistance, providing insights into treatment failures in specific patient populations, and advancing precision therapies. By incorporating patient-specific variations, organoid models offer a more accurate representation of clinical outcomes, accelerating cancer research and therapeutic development.
Exploring the LAR-Positive SUM185PE Cell Line in Triple-Negative Breast Cancer
The SUM185PE cell line represents a luminal androgen receptor (LAR)-positive subtype of triple-negative breast cancer (TNBC), which is characterized by a reliance on androgen receptor (AR) signaling despite lacking estrogen receptor (ER), progesterone receptor (PR), and HER2 expression. One of its key oncogenes is PIK3CA, a frequently mutated gene that activates the PI3K/Akt/mTOR pathway, promoting tumor cell survival and growth. SUM185PE cells exhibit luminal gene expression patterns, with high levels of FOXA1, XBP1, and KRT18, distinguishing them from basal-like TNBC subtypes. This subtype shows high sensitivity to AR antagonists like bicalutamide, suggesting a potential therapeutic avenue for AR-driven breast cancers. Additionally, SUM185PE cells display vulnerabilities in mTORC1 signaling, making them susceptible to PI3K/mTOR inhibitors as combination therapy. Compared to other TNBC subtypes, the LAR subtype has lower relapse-free survival, emphasizing the aggressive nature of AR-driven tumors. Understanding the oncogenic drivers in SUM185PE cells is crucial for developing targeted therapies that exploit AR and PI3K/mTOR dependencies in this subset of TNBC.
At Altogen Labs, based in Austin, Texas, offers a comprehensive platform for breast cancer research through specialized xenograft models. These models are designed to study tumor progression, therapeutic efficacy, and biological mechanisms in HER2-positive and other breast cancer subtypes. Researchers can investigate tumor growth dynamics and response to novel treatments using various assessment methods, such as Tumor Growth Delay (TGD) and Tumor Growth Inhibition (TGI). These models support flexible dosing strategies, including intravenous, oral gavage, or intratumoral injections, allowing for the evaluation of different treatment regimens. Breast cancer xenograft models at Altogen Labs, established via subcutaneous or orthotopic implantation, provide a detailed in vivo system to study tumor growth, metastasis, and drug resistance. Advanced analytical techniques are utilized, such as, immunohistochemistry, gene expression profiling, and fluorescence-based imaging for in vivo tumor monitoring. These approaches enable in-depth analysis of tumor characteristics and therapeutic responses. Whether exploring estrogen receptor-positive, estrogen receptor-negative, or aggressive HER2-positive tumors, Altogen Labs offers the specialized models and expertise needed to drive your oncology research forward.
