HCC1954 Xenograft Model
The ACS approximates for 2019, United States breast cancer rates are: Around 268,600 new invasive breast cancer cases, 62,930 new cases of breast cancer in situ (CIS, meaning non-invasive or early stage) and 41,760 fatalities attributed to breast carcinoma. Recently data shows the past few years have demonstrated a small increase in the rates of breast cancer (+0.4%/year). The HCC1954 cell line was derived from the stage II breast cancer of a 61yo East Indian female diagnosed with ductal carcinoma.
The HCC1954 model has been used in many breast cancer research studies. Beyer et al. (Cancer Research, 2011) used the HCC1954 model to study how to improve the efficacy of monoclonal antibody therapy in breast cancer using JO-1 (Junction opener 1), a small recombinant adenovirus protein derived from serotype 3. Results showed JO-1 binds to DSG2 and combination of JO-1 with Erbitux (cetiximab) or trastuzumab (Herceptin) increased therapeutic efficacy in part due to improved target access. In 2016, Xiong et al. published an Oncotarget study using HCC1954 cells to study CD147 knockdown in improving trastuzumab, a HER2 antibody, efficacy treatment in breast cancer. Results demonstrated that suppressing CD147 (knockdown) with trastuzumab treatment resulted in increased apoptosis (Caspase-3 cleaving and PARP marker) and decreased MAPK and Akt phosphorylation. This data has implications for trastuzumab antibody drug resistance/sensitivity for treating breast cancer. Finally, He et al. published a 2017 Science Reports study using HCC1954 to evaluate androgen receptor targeting in HER2 expressing brast cancer. Results demonstrated using Enzalutamide, an anti-androgen agent, with trastuzumab successfully decreased cancer growth and Ki67 staining. The HCC1954 cell line is used to create the CDX (Cell Line Derived Xenograft) HCC1954 xenograft mouse model. The HCC1954 xenograft model has been used to investigate breast carcinoma treatments and therapies (cetuximab, JO-1, trastuzumab, etc.).
HCC-1954 Orthotopic And Metastatic Xenograft Model: Download ![]()
Metastatic HCC1954 Xenograft Model
The metastatic HCC1954 model is used to study the dissemination of HER2-positive breast cancer cells to distant organs preclinically. By orthotopically implanting HCC1954 cells into the mammary fat pad of immunodeficient mice, researchers can observe spontaneous metastasis, particularly to the brain. This model has been instrumental in identifying molecular features associated with brain tropism and in evaluating therapeutic strategies targeting metastatic lesions. For instance, studies have demonstrated that HCC1954 cells can develop brain metastases following primary tumor resection, mimicking clinical scenarios of metastatic progression. Additionally, the model has been used to investigate the role of natural killer (NK) cells in controlling metastatic outgrowth, revealing that NK cell depletion facilitates the expansion of HCC1954 metastatic cells in the brain.
Advancing Breast Cancer Studies with Orthotopic HCC1954 Models
The orthotopic HCC1954 model is used in nonclinical experiments to study HER2-positive breast cancer by implanting HCC1954 cells into the mammary fat pad of immunodeficient mice. This approach replicates the tumor’s natural environment, providing insights into tumor behavior and treatment responses. Researchers utilize this model to evaluate therapies targeting HER2 overexpression, such as trastuzumab and cetuximab. The model has been instrumental in assessing the efficacy of various therapeutic agents, including monoclonal antibodies and small molecule inhibitors. Studies have demonstrated its utility in testing novel treatments and understanding resistance mechanisms in HER2-positive breast cancer.
Case Study: HCC1954 Cells Reveal Cholesterol-Driven ErbB2 Regulation and Therapeutic Vulnerabilities
A study conducted by Zhang J, et al., published by Cell Communication and Signaling journal investigated the role of membrane cholesterol in regulating ErbB2 levels and therapeutic responses in ErbB2-positive breast cancer. Using the HCC1954 cell line, along with SKBR3 and AU565, researchers found that cholesterol abundance stabilizes ErbB2 on the cell surface, while cholesterol depletion enhances its internalization and degradation. Compared to SKBR3 and AU565, HCC1954 cells exhibited lower cholesterol levels and increased intracellular ErbB2 localization. Treatment with the cholesterol-lowering drug lovastatin disrupted membrane rigidity and sensitized HCC1954 cells to the ErbB2 inhibitor lapatinib, leading to enhanced tumor suppression in both in vitro and in vivo models. Mechanistically, lovastatin promoted ErbB2 degradation via endocytosis, reducing its oncogenic signaling. In HCC1954 xenografts, the combination of lovastatin and lapatinib significantly inhibited tumor growth compared to lapatinib alone. These findings suggest that targeting cholesterol metabolism could enhance ErbB2-targeted therapies, providing a potential combinatorial strategy for treating ErbB2-positive breast cancer.
HCC1954 Model for Advancing HER2-Targeted Immunotherapy in Resistant Breast Cancer
Another study by Li H, et al., published by American Journal of Cancer Research, explored strategies to overcome trastuzumab resistance in HER2-positive breast cancer using third-generation anti-HER2 chimeric antigen receptor (CAR)-T cells alone and in combination with PD1 blockade. The HCC1954 cell line, known for its intrinsic resistance to trastuzumab, was a key model in both in vitro and in vivo experiments. Anti-HER2 CAR-T cells specifically targeted HER2-positive HCC1954 and BT474 cells, leading to increased secretion of IL-2 and IFN-γ, which was further enhanced by PD1 blockade. Cytotoxicity assays revealed that anti-HER2 CAR-T cells effectively eliminated HCC1954 cells, and the addition of anti-PD1 antibody significantly boosted this effect. In xenograft models, injection of anti-HER2 CAR-T cells led to a marked reduction in HCC1954 tumor growth, which was further inhibited when combined with PD1 blockade. Mechanistically, PD1 blockade enhanced CAR-T cell persistence and function, preventing T-cell exhaustion and improving therapeutic outcomes. These results highlight the potential of combining CAR-T therapy with immune checkpoint inhibitors to treat trastuzumab-resistant HER2-positive breast cancer, with HCC1954 serving as a crucial model system for developing such targeted therapies.
Key Oncogenes in HCC1954: Understanding HER2, Integrins, and Cadherins
HCC1954 is a HER2-positive breast cancer cell line characterized by high invasiveness and resistance to trastuzumab therapy. The primary oncogene driving its aggressive behavior is HER2 (ErbB2), which amplifies cell proliferation and survival through the PI3K/AKT and MAPK/ERK pathways. Another critical oncogene in HCC1954 is β1 integrin (ITGB1), a key regulator of adhesion and migration that contributes to trastuzumab resistance and promotes metastasis. Studies indicate that HER2 and β1 integrin exhibit crosstalk, enhancing cancer cell motility and therapy resistance. E-Cadherin (CDH1), typically associated with epithelial integrity, is also highly expressed in HCC1954, suggesting an intermediate epithelial–mesenchymal phenotype that supports both adhesion and migration. Additionally, CD166 (ALCAM), an immunoglobulin superfamily member, is highly expressed, reinforcing tumor invasiveness and therapy resistance. The interplay of these oncogenes defines HCC1954 as a robust model for studying HER2-positive breast cancer progression and drug resistance mechanisms.
Chemotherapy: Radio-sensitization in HER2-Positive Cancers
HCC1954 is a HER2-overexpressing breast cancer cell line widely used to study targeted cancer therapies and resistance mechanisms. As a model for aggressive HER2-positive tumors, it helps researchers understand how specific treatments influence tumor behavior. Tucatinib, a HER2-directed tyrosine kinase inhibitor, has shown potential to enhance the effects of radiation therapy, leading to reduced cell proliferation and survival. However, sensitivity to tucatinib varies, particularly in cancer cells with additional mutations like PIK3CA, which can contribute to drug resistance. Combining tucatinib with a PI3K inhibitor has been shown to improve treatment response in such cases. Additionally, the sequence of treatment plays a role, with radiation followed by tucatinib producing stronger effects. These findings support the use of combination therapies to overcome resistance and improve outcomes, especially in cancers prone to metastasizing to the brain.
Chromosomal Rearrangements in HCC1954 Breast Cancer Cells
The HCC1954 breast cancer cell line exhibits a highly complex karyotype characterized by a pseudo-tetraploid genome with an average of 92 chromosomes per cell. Spectral karyotyping (SKY) reveals extensive chromosomal rearrangements, including interchromosomal and intrachromosomal translocations affecting nearly all chromosomes. Among the most notable genomic alterations are translocations involving chromosomes 4, 5, 8, 9, 11, and 18, leading to gene fusions and truncations. Key oncogenic genes such as MRE11A and NSD1 are disrupted, impacting DNA repair mechanisms and transcription regulation. Additionally, frequent rearrangements on chromosome 8, particularly in the 8q24 region, highlight a known recombination hotspot associated with cancer susceptibility. Fluorescence in situ hybridization (FISH) and long-range PCR confirm several of these genomic breaks, emphasizing the extensive genomic instability of HCC1954. This karyotypic complexity reflects the aggressive nature of HER2-positive breast cancer and provides a valuable model for studying chromosomal rearrangements in tumorigenesis.
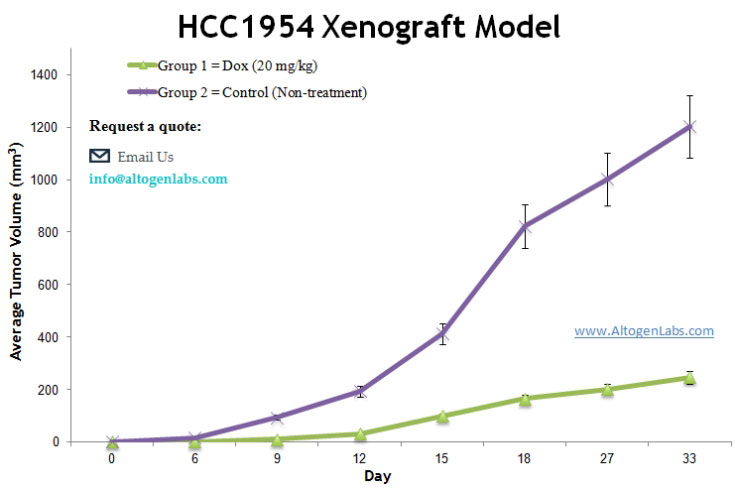
Basic Study Design
- HCC1954 cells are maintained in exponential growth phase under aseptic conditions.
- Cells are trypsinized and cell count viability is determined using a trypan blue exclusion assay (99% of cell viability is required). HCC1954 cell suspension adjusted to appropriate density.
- Each mouse is singly subcutaneously injected into the right flank with 2-4 x 106 cells in 100 µL of a Matrigel – HCC1954 cell suspension.
- The injection sites are palpated up to three times weekly until tumors are established to an average size of 150-200 mm3 as measured via digital calipers.
- Animals are randomized into treatment groups. Administration of test compound is performed according to the preestablished treatment schedule.
- Mice weights are measured and recorded 2-3 times weekly; tumors are measured and recorded daily.
- End of study is reached when tumor size reaches 2,000 mm3 or the predetermined size limit per approved IACUC protocol.
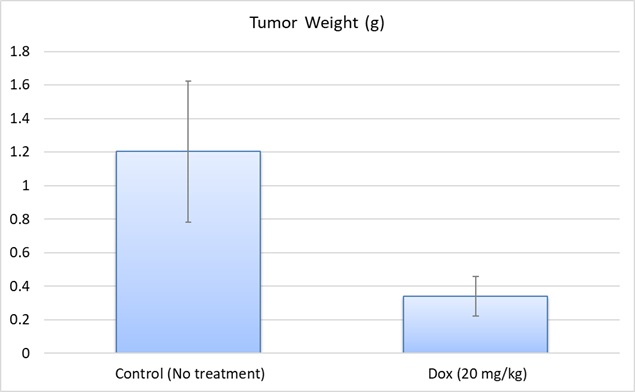
- Final necropsy and tissue collections are performed for appropriate downstream analysis. Tumors are excised, weighed and documented by digital imaging. Tumors and tissues can be stabilized in RNA-Later reagent, snap frozen in LN2 or prepared for histology.
HCC-1954 Orthotopic And Metastatic Xenograft Model: Download ![]()
