Breast cancer affects 12% of women worldwide and is the most common invasive cancer type in women. In 2008 it caused almost half a million deaths worldwide which demonstrates the need for an improvement in treatment and breast cancer research. The ZR-75-1 xenograft model has been used in many breast cancer studies. In 1997 ZR-75-1 xenografts were used to evaluate the use of tamoxifen on breast cancer (Breast Cancer Research and Treatment, Cameron et al.). Results demonstrated that tamoxifen treatment does not affect necrosis but does increase apoptosis and decrease proliferation in ER negative (but not ER positive) cell lines. Tamoxifen today is a well-known anticancer treatment, although its use in early breast cancer was not established until 1998. A tamoxifen study in 1998 (Couillard et al., Cancer Research) also used the ZR-75-1 xenograft model to look at combination treatment with EM-800 antiestrogens. Data demonstrated that in the presence of estrogen (supplemented in ovariectomized (OVX) mice), tamoxifen treatment results in tumor growth stimulation whereas combination treatment with EM800 resulted in a synergistic decrease in tumor size. This has clinical relevance for predicting tamoxifen response based on estrogen levels as well as a potential method for amplifying the anticancer effect of tamoxifen. Kudoh et al. published a Cancer Research study (2002) using the ZR-75-1 cell line to investigate the role of Bag1 proteins in breast cancer. Bag1 proteins are known to interact with Hsp70 and regulate proliferation, stress response and apoptosis and are upregulated in breast cancer. Data demonstrated that Bag1 (and Bag1L) proteins increased survival in vitro and in vivo, providing evidence for the study of Bag1L for cancer treatment.
ZR-75-1 Orthotopic And Metastatic Xenograft Model: Download ![]()
ZR-75-1 Cell Line
The ZR-75-1 cell line was isolated from the mammary gland tissue of a 63-year-old White female patient diagnosed with ductal breast carcinoma. This epithelial cell line is characterized by its ability to grow as adherent monolayers and is widely used in breast cancer research due to its relevance to human disease. ZR-75-1 cells exhibit estrogen receptor (ER) positivity, making them an ideal model for studying hormone-responsive breast cancer. They also express other key markers such as progesterone receptors and HER2, allowing for the investigation of therapies targeting these pathways. The ZR-75-1 cell line provides a reliable in vitro platform to explore tumor biology, including cell proliferation, invasion, and response to various treatment modalities. It is frequently utilized for drug screening, including hormonal therapies, targeted therapies, and chemotherapy. Additionally, the ZR-75-1 cell line supports studies of molecular mechanisms involved in breast cancer metastasis and drug resistance. As an established model in cancer research, ZR-75-1 remains crucial for advancing the understanding of breast cancer pathophysiology and treatment.
Targeting Glycolysis in Chemotherapy: The Role of DCXR in ZR-75-1 Breast Cancer Cells
The ZR-75-1 breast cancer cell line serves as a crucial model for studying the oncogenic role of dicarbonyl/L-xylulose reductase (DCXR) in tumor progression. DCXR is significantly upregulated in breast cancer tissues and enhances glycolysis, fueling cell proliferation and cell cycle progression. Experimental knockdown of DCXR in ZR-75-1 cells led to suppressed proliferation, reduced glycolytic activity, and cell cycle arrest at the G1 phase, reinforcing its role as a driver of cancer cell metabolism. Conversely, DCXR overexpression in breast cancer cells promoted glycolysis and accelerated the S-phase transition, highlighting its oncogenic potential. Further, in vivo xenograft models using ZR-75-1 cells demonstrated that DCXR silencing reduces tumorigenicity, making it a promising therapeutic target. The study also revealed that the glycolysis inhibitor 2-deoxy-D-glucose (2-DG) effectively blocked the pro-tumorigenic effects of DCXR, suggesting a potential metabolic intervention strategy. Understanding the metabolic dependencies of ZR-75-1 cells through DCXR provides new insights into breast cancer treatment strategies focused on disrupting cancer cell energy metabolism.
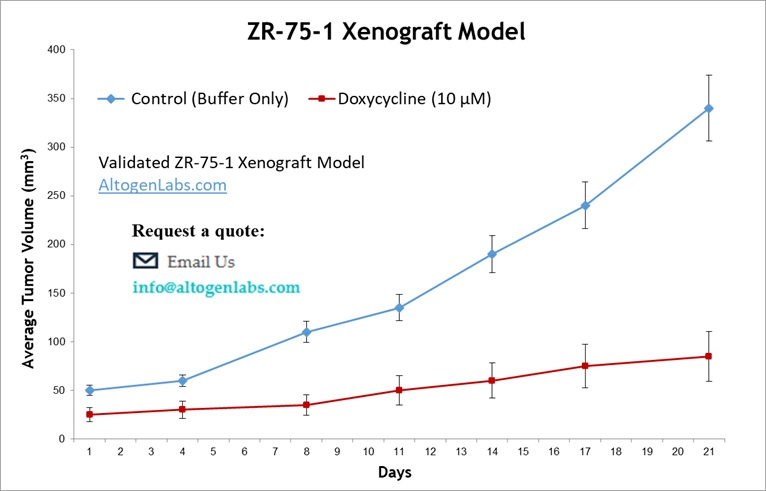
Exploring Treatment Efficacy with the Subcutaneous ZR-75-1 Model
The subcutaneous ZR-75-1 model is a commonly used preclinical model for studying human breast cancer in a non-invasive setting. In this model, ZR-75-1 cells, derived from a human breast adenocarcinoma, are injected into the flank of immunocompromised mice. This implantation method results in the formation of tumors that can be easily monitored for growth and response to treatments. The subcutaneous location allows for straightforward measurements of tumor size and volume, making it a valuable model for high-throughput drug screening and therapeutic assessments. Researchers often use the subcutaneous ZR-75-1 model to evaluate the effects of chemotherapy, hormone therapies, and targeted treatments. Though less reflective of the tumor microenvironment compared to orthotopic models, this model provides important insights into tumor biology and the potential efficacy of cancer therapies. The subcutaneous ZR-75-1 model is widely recognized for its reproducibility and convenience, making it essential for preclinical breast cancer research.
Studying Metastasis with the ZR-75-1 Metastatic Model
The metastatic ZR-75-1 model is used in nonclinical research for studying the metastatic progression of human breast cancer. In this model, ZR-75-1 cells, derived from a human breast adenocarcinoma, are injected into immunocompromised mice, typically via the tail vein, to simulate hematogenous dissemination of cancer cells. This model allows researchers to track the spread of cancer to distant organs such as the lungs, liver, and bones, closely mimicking the metastatic process observed in human breast cancer patients. The metastatic ZR-75-1 model is widely used to evaluate the effectiveness of anti-metastatic therapies and to understand the molecular mechanisms underlying tumor dissemination. Its ability to assess both primary tumor growth and secondary metastatic lesions makes it invaluable in cancer research. The model also supports studies of tumor-host interactions in distant organs and the development of resistance to therapy. Its reproducibility and ability to simulate a range of metastatic events make the metastatic ZR-75-1 model an essential platform for evaluating therapeutic strategies aimed at reducing metastasis in breast cancer.
Evaluating Novel Therapies Using the ZR-75-1 Orthotopic Breast Cancer Model
The orthotopic ZR-75-1 model is a widely used preclinical model for studying human breast cancer in vivo. Derived from a human breast adenocarcinoma, ZR-75-1 cells are implanted into the mammary fat pad of immunocompromised mice to closely replicate the tumor microenvironment seen in patients. This model allows for the evaluation of tumor growth, metastasis, and therapeutic responses in a setting that mirrors the natural progression of breast cancer. Researchers commonly use the orthotopic ZR-75-1 model to assess the efficacy of novel drug candidates, including hormonal therapies, targeted therapies, and combination treatments. The model’s ability to mimic human breast cancer characteristics makes it invaluable for preclinical testing and biomarker discovery. Additionally, it serves as a platform for understanding tumor-host interactions, such as angiogenesis and immune response. Its ability to facilitate both localized and metastatic studies provides a comprehensive method for evaluating treatment strategies across different stages of cancer progression.
Immuno-oncology Xenograft Models by Altogen Labs
Altogen Labs is a leading preclinical research organization specializing in the evaluation of innovative pharmacological and biological therapies, including cancer treatments, medical compounds, vaccines, cosmetics, and natural products. With a team of skilled scientists, the company offers state-of-the-art laboratory services, employing cutting-edge technologies to drive oncology research and expedite drug development. Altogen Labs is known for its specialized immuno-oncology services, utilizing humanized and immunodeficient rodent models engrafted with peripheral blood mononuclear cells (PBMC), CD34+ hematopoietic stem cells, and induced pluripotent stem cells (iPSC) to assess immune responses, drug efficacy, and toxicity. One of the company’s key strengths is its extensive portfolio of over 100 in-house validated xenograft models, including Cell Line Derived Xenografts (CDX), patient-derived xenografts (PDX), in vitro patient-derived cell cultures (PDC), and patient-derived organoids (PDOrg), providing clinically relevant platforms for predicting drug efficacy. Additionally, Altogen Labs conducts thorough toxicity studies, assessing acute, sub-chronic, and chronic toxic effects to ensure the safety and long-term tolerability of compounds.
Altogen Labs provides an extensive range of laboratory services, including the ZR-75-1 xenograft model, to support comprehensive cancer research. The ZR-75-1 model, in particular, is highly valuable for studying estrogen receptor-positive breast cancer, offering a relevant and reliable platform for assessing treatment efficacy. This cell line, derived from a human breast adenocarcinoma, closely mirrors the tumor’s biological behavior and provides insights into the molecular pathways of cancer. In addition to tumor growth and metastasis studies, Altogen Labs offers the development of genetically engineered cell lines for protein overexpression or RNAi-based cell lines for long-term gene silencing, which are essential for investigating the roles of specific proteins and gene products in cancer progression. Researchers can also perform quantitative gene expression analysis using RT-PCR for mRNA and protein expression analysis with the WES system (ProteinSimple), ensuring precision in molecular target evaluation and treatment outcome studies.
ZR-75-1 Xenografts Reveal PI3K Inhibition as a Key Strategy Against CDK4/6 Therapy Resistance
A study conducted by O’Brien, et al., published by Breast Cancer Research journal, investigates the mechanisms underlying acquired resistance to CDK4/6 inhibitors in ER+/HER2− breast cancer and explores therapeutic strategies to overcome this challenge. Through the development of preclinical models, the researchers identified that resistance is frequently driven by the loss of Rb or a diminished reliance on Rb signaling, resulting in cross-resistance to CDK4/6 inhibitors. Despite this resistance, PI3K/mTOR signaling remains persistently activated, presenting a viable therapeutic target. Notably, ZR-75-1 xenografts, engineered to develop resistance to alpelisib and fulvestrant, played a pivotal role in demonstrating that PI3K inhibition effectively halts tumor progression, even in CDK4/6-resistant models. Treatment with the p110α-selective PI3K inhibitor, alpelisib, induced robust tumor regression in both PIK3CA-mutant and wild-type ER+/HER2− breast cancers, underscoring the therapeutic potential of PI3K pathway blockade. Furthermore, the addition of CDK4/6 inhibitors to PI3K:ER-targeted therapy successfully reversed resistance in tumors that had progressed on PI3K inhibition alone, highlighting the interdependency of these signaling pathways. These findings provide strong preclinical support for the clinical evaluation of PI3K inhibitors, such as alpelisib, in patients with ER+/HER2− breast cancer who progress on CDK4/6-based therapies. Moreover, the data suggest that upfront triple combination therapy, simultaneously targeting PI3K, CDK4/6, and ER; may serve as a powerful strategy to delay or even prevent the emergence of therapeutic resistance. The study underscores the critical role of ZR-75-1 xenografts in modeling resistance and optimizing next-generation treatment approaches for endocrine-resistant breast cancer.
The Role of ZR-75-1 in Breast Cancer Research Using 3D Models
Nonclinical breast cancer research has greatly benefited from three-dimensional (3D) culture models, including organoids, which closely mimic the tumor microenvironment compared to traditional two-dimensional (2D) models. The ZR-75-1 breast cancer cell line is particularly valuable in these studies, providing insights into luminal-type breast cancer biology. 3D models and organoids allow researchers to study the interactions between tumor cells and the extracellular matrix (ECM), revealing critical transcriptional changes that drive tumor progression, epithelial-to-mesenchymal transition (EMT), and drug resistance. Unlike conventional 2D cultures, organoids derived from ZR-75-1 cells better replicate in vivo tumor characteristics, allowing researchers to use them for personalized medicine and drug discovery. These advanced models help identify novel therapeutic targets and improve our understanding of breast cancer heterogeneity, offering new opportunities for developing more effective treatments. By preserving the structural and genetic complexity of patient tumors, organoids provide a more accurate platform for testing targeted therapies and predicting treatment responses. As research continues to refine these models, the combination of ZR-75-1 cells and organoid technology holds great promise for revolutionizing breast cancer treatment and precision medicine.
Metabolic Signatures of ZR-75-1 Oncogenes in Tumor Growth
ZR-75-1 is a hormone receptor-positive breast cancer cell line that exhibits a unique metabolic phenotype driven by its oncogenic profile. Unlike highly proliferative triple-negative breast cancer cells, ZR-75-1 cells display a stronger dependence on glycolysis rather than oxidative phosphorylation. This metabolic reliance suggests that oncogenic signaling within these cells prioritizes biosynthetic pathways fueled by glycolytic intermediates over mitochondrial respiration. Notably, ZR-75-1 cells demonstrate resistance to transaminase inhibition but exhibit high sensitivity to glutamate dehydrogenase (GDH) inhibition, aligning with their lower proliferation rates. This metabolic pattern reflects the cell line’s role as a model for less aggressive breast cancer subtypes. The metabolic plasticity of ZR-75-1 underscores the adaptability of hormone receptor-positive cancers, influencing therapeutic strategies targeting metabolic vulnerabilities. Understanding its oncogene-driven metabolic landscape may lead to more precise treatment options for similar breast cancer subtypes.
Basic Study Design:
- ZR-75-1 cells are maintained in exponential growth phase under aseptic conditions.
- Cells are trypsinized and cell count viability is determined using a trypan blue exclusion assay for 99% cell viability.
- Each mouse is subcutaneously injected into the left flank with 2 – 4 million ZR-75-1 cells in 100-200 µL of a Matrigel-ZR-75-1 cell suspension.
- The injection sites are palpated up to three times weekly until tumors are established to an average size of 150-250 cubic mm.
- Animals are randomized into treatment groups. Administration of test compound is performed according to the treatment schedule.
- Mice weights are measured and recorded 2 times weekly; tumors are measured and data recorded daily.
- End of study is reached when tumor size reaches at 45 days or 2,000 cubic mm tumor volume.
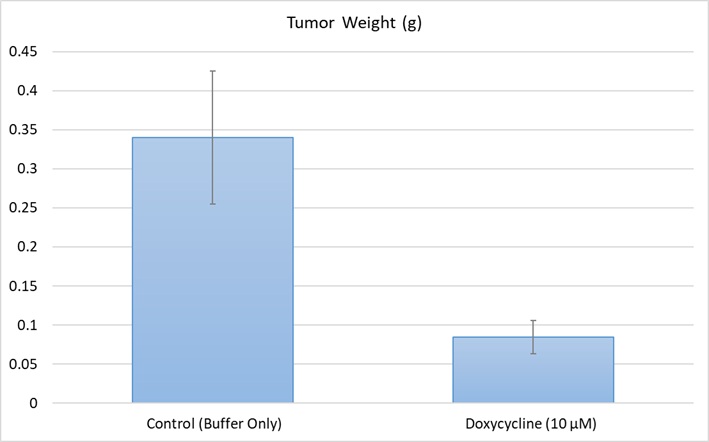
- Tumors are excised, weighed and documented by digital imaging. Tumor tissues are stabilized in RNA-Later, or snap frozen in LN2 or prepared for histology.
