Daudi Xenograft Model
Lymphomas are a group of blood cancers that affect lymphocytes, a white blood cell type. Symptoms include fever, sweats, itching, weight loss, fatigue and enlarged lymph nodes. Risk factors include autoimmune diseases, HIV/AIDS, the Epstein-Barr virus, and smoking tobacco. The two main types are Hodgkin’s lymphoma and non-Hodgkin lymphoma. The five-year survival rate in the US is 85%. Burkitt’s lymphoma affects B lymphocytes and is commonly associated with malaria endemic regions, AIDS/HIV and the Epstein-Barr virus. It is often a childhood cancer. The Daudi cell line was first isolated in 1967 by E and G Klein from the peripheral blood of a 16 year old Black male diagnosed with Burkitt’s lymphoma. Daudi cells have since been used in various research studies. A 2019 Blood Journal study (Chang et al.) used the Daudi cell line to test the efficacy of a recombinant RNase Ranpirnase combined with an anti-CD-74 humanized antibody (2L-Rap-hLL1-γ4P). Treatment data demonstrates that the recombinant immunotoxin reduced in vitro and in vivo tumor growth, supporting further study for its use against CD74 positive tumors. A 2005 Clinical Cancer Research study by Michel et al. used Daudi xenografts to study radionuclide-conjugated antibodies. The radionuclides emit low-energy electrons, and when conjugated to an antibody are able to radiate targeted cells while causing minimal irradiation damage to surrounding tissue. Results demonstrated that xenograft tumors were successfully treated with this technique, supporting it as an effective therapy against micrometastatic cancer. Finally, a 2019 study by Xuan et al. (Blood Journal) utilized the Daudi model in order to study the efficacy of using interferon alpha (IFNα)/anti-CD20 antibody (rituximab) fusion protein as a method for overcoming rituximab-resistant CD20+ tumors. Data demonstrated treatment with the fusion protein resulted in tumor eradication. The Daudi cell line is used to create the xenograft mouse model.
The Daudi cell line has been widely used in research as a model system for studying various aspects of B cell biology, including immunoglobulin production, antigen processing and presentation, and antibody-mediated cytotoxicity. Additionally, the Daudi cell line has been used to investigate the mechanisms of action of potential therapeutic agents for lymphomas and other cancers. The Daudi xenograft model has been used extensively as a model for studying the mechanisms of leukemogenesis. The Daudi cell line is available from various cell banks and can be cultured under standard cell culture conditions. It has been used in numerous studies investigating the genetic and molecular basis of Burkitt’s lymphoma and other B cell lymphomas.
Basic Study Design
- Daudi cells are maintained in exponential growth phase under aseptic conditions.
- Cells are trypsinized and cell count viability is determined using flow cytometry or a trypan blue exclusion assay (98-99% of cell viability is required). Daudi cell suspension is adjusted to appropriate density.
- Each mouse is singly subcutaneously injected into the right flank with 106 cells in 150-200 µL of a Matrigel-Daudi cells suspension.
- The injection sites are palpated up to three times weekly until tumors are established to an average size of 50-150 mm3 as measured by digital calipers.
- Animals are randomized into treatment groups. Administration of test compound is performed according to the pre-established treatment schedule.
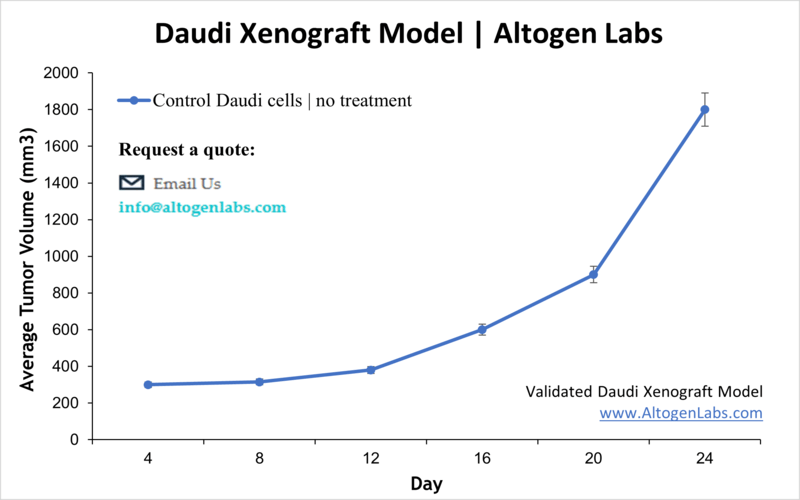
- Mice weights are measured and recorded 3 times weekly; tumors are measured and recorded daily.
- End of study is reached when tumor size reaches 2,000 mm3 or the predetermined size limit per approved IACUC protocol.
- Final necropsy and tissue collections are performed for appropriate downstream analysis. Tumors are excised, weighed and documented by digital imaging. Tumors and tissues can be stabilized in RNA-later reagent, snap frozen in LN2 or prepared for histology.
